Female Fertility Services
In Vitro Fertilization (IVF)
In Vitro Fertilization (IVF) is the oldest Artificial Reproductive Technology (ART) procedure and still the most frequently used. The term “in vitro” refers to fertilization outside the body. Originally designed to bypass damaged fallopian tubes, new applications for IVF quickly developed for male factor infertility, endometriosis, unexplained infertility and other conditions. For most reproductive issues, research has clearly demonstrated that IVF, and its variations, hold the greatest promise of successful pregnancy per month, more than any other intervention. Much of this success is due to the acceleration of what occurs in natural conception. Couples with normal fertility do not conceive every month but will conceive when the “right” egg is produced. With IVF, many more eggs can usually be produced in one month, which increases the chance that one or more of them are normal. Further, assisted insemination and confirmation of fertilization are significant achievements only available with in vitro observation. SART 2022 Preliminary Report | SART 2021 Final Report A routine IVF cycle of treatment consists of daily fertility medications, injection to trigger egg maturation, egg retrieval, insemination, and culture of resulting embryos, and finally, transfer of the most developed embryos into the woman’s uterus. Pregnancy testing is completed less than 2 weeks later, so the entire process is similar in length to one natural menstrual cycle. Many couples are appropriately concerned about the cost of IVF technologies. Much of the apprehension seems to arise from information found on the internet, rather than for a specific couple. IVF costs vary depending on a patient’s particular needs and will best be determined after the initial appointment when all of your medical records and testing have been reviewed and discussed. In Vitro Fertilization may not be right for every couple, but rest assured that honest counseling at NewLIFE will provide patients with all viable options. Should patients decide IVF is right for them, the staff will happily discuss how costs are lower at NewLIFE in comparison to the national average. There are many advantages to receiving fertility care in smaller communities like Pensacola, Mobile, Panama City, and Dothan.Intrauterine Insemination (IUI)
Intrauterine Insemination (IUI) allows sperm, prepared from a semen sample, to be introduced into the uterus through the cervix using a thin plastic catheter. By preparing the semen sample, sperm can be concentrated. The concentrated sperm is placed into the upper uterine cavity, increasing the number of viable sperm that reach the end of the fallopian tubes and the eggs. While it is not believed to enhance how the sperm fertilize, it may increase the chance of fertilization by increasing the interaction between the capable sperm and the egg. IUI is commonly used for mild male fertility factors and for unexplained infertility. Testing for male infertility has advanced recently allowing a better prediction of success with various treatments. Notably, IUI used alone has not been shown to be effective for most cases of infertility. Therefore, IUI is most often used in combination with fertility medications that increase the number of eggs available for fertilization. More severe cases of male infertility and combinations of fertility problems will be best served by in vitro fertilization (IVF).Pre-implantation Genetic Testing (PGT)
The field of human reproduction is constantly advancing, bringing tangible benefits to patients. Pre-implantation Genetic Testing (PGT) is used to help select for transfer of only the most healthy embryos. Routine in vitro fertilization (IVF) continues to result in the placement of embryos into the uterus that are not genetically intact and fail to produce a pregnancy. Further, some of these abnormal embryos will result in transiently positive pregnancy tests and/or early miscarriages. This approach, using PGT, has been shown to reduce the chance of miscarriage. In fact, it appears to improve the successful reproductive chances for some older women who have experienced pregnancy losses associated with genetically abnormal conceptions. Finally, this may be a way of reducing the negative impact of a woman’s age on her pregnancy outcome. In 2010, NewLIFE was the first to implement this breakthrough technology on the Florida/Alabama Gulf Coast. The successes have been astoundingly positive and more patients are taking advantage of this service. As the experience has expanded, PGT appears to improve pregnancy rates for most infertility problems and is likely to become a common component of IVF cycles. Currently, embryos tested by PGT must be cryopreserved while waiting for test results. Surprisingly, this postponement of embryo transfer is showing evidence of better implantation than even fresh embryo transfers. Part of this progress was delivered by improvements in cryopreservation and thawing techniques. The technology has arrived at last to improve the chances and restore confidence for women who have suffered repeated pregnancy losses. If you have experience with pregnancy loss, please know there is hope. If you know someone that has experienced this as well let them know that help is available. Pre-implantation Genetic Testing near MeSurgery for Fertility Preservation
Laparoscopy
Laparoscopy (“band-aid surgery”) is the method of choice when surgery is needed to evaluate and to treat infertility that is associated with conditions such as endometriosis, blocked fallopian tubes, and adhesions. This minimally invasive and outpatient surgical approach offers a very short recovery and proven successful outcomes. The Fellowship-trained and Board Eligible/Certified physicians at NewLIFE are uniquely experienced in fertility-preserving laparoscopy. While surgery is rarely a first choice, patients should feel confident in their surgeon’s abilities and training. Patients can read about personal experiences of other women who had this surgery for infertility on our “People Sharing Their NewLIFE Experiences” webpage. Endometriosis is a common condition, more common in a population of infertile women. Symptoms do not reliably predict its presence, but combinations of findings can raise suspicions. Fortunately, well-designed clinical trials support laparoscopic surgery to be an effective intervention. Patients who feel that endometriosis is their impediment to successful conception are encouraged to learn more. Our Board-Certified Reproductive Endocrinologists are uniquely trained to address this problem. Dr. Ripps achieved international acclaim for his pioneering contributions and research to better understand and treat endometriosis and its associated consequences.
Endometriosis is a common condition, more common in a population of infertile women. Symptoms do not reliably predict its presence, but combinations of findings can raise suspicions. Fortunately, well-designed clinical trials support laparoscopic surgery to be an effective intervention. Patients who feel that endometriosis is their impediment to successful conception are encouraged to learn more. Our Board-Certified Reproductive Endocrinologists are uniquely trained to address this problem. Dr. Ripps achieved international acclaim for his pioneering contributions and research to better understand and treat endometriosis and its associated consequences.
Tubal Ligation Reversal
For women, a previous sterilization by a tubal ligation does not have to be permanent!
With more than 30 years of tubal ligation reversal experience, NewLIFE has an established record for surgical success and healthy pregnancies after Tubal Ligation Reversal (TLR). Fellowship training to increase experience and Board Certification as Reproductive Surgeons are credentials that set the standard. These should be the most valuable criteria when seeking and selecting a surgeon for TLR.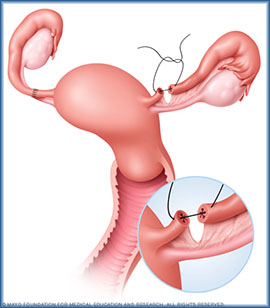 A pre-surgical consultation and testing will help assure that TLR is the correct choice and that a successful pregnancy is likely. This procedure for women yields excellent surgical results with re-opening of one or both tubes in 90% of cases. Though the woman’s age is an important factor, for women with confirmation of open tubes, the NewLIFE experience reports a pregnancy rate greater than 70%.
The procedure is planned as “outpatient” or “same-day surgery” and patients are able to return to their routine activities quickly. Providing low-cost reversal of tubal ligation is a specialty of this practice. Most patients have TLR completed for predetermined, discounted fees, *negotiated to include the surgery, anesthesia, and facility fees.
As with patients who “vacation” in Pensacola, Florida to receive fertility treatments, a successful reversal procedure can be completed conveniently, recovering with your “toes in the sand” before returning home. Florida locations are ideal to accommodate out-of-town patients. Delightful hotels are conveniently close and many couples vacation at the world’s most beautiful beaches during their visits.
Patients can read about personal experiences of other women who had this surgery for infertility on our “People Sharing Their NewLIFE Experiences” webpage.
*Actual cost may vary for some patients based on location, and an individual’s need for medications and other services.
A pre-surgical consultation and testing will help assure that TLR is the correct choice and that a successful pregnancy is likely. This procedure for women yields excellent surgical results with re-opening of one or both tubes in 90% of cases. Though the woman’s age is an important factor, for women with confirmation of open tubes, the NewLIFE experience reports a pregnancy rate greater than 70%.
The procedure is planned as “outpatient” or “same-day surgery” and patients are able to return to their routine activities quickly. Providing low-cost reversal of tubal ligation is a specialty of this practice. Most patients have TLR completed for predetermined, discounted fees, *negotiated to include the surgery, anesthesia, and facility fees.
As with patients who “vacation” in Pensacola, Florida to receive fertility treatments, a successful reversal procedure can be completed conveniently, recovering with your “toes in the sand” before returning home. Florida locations are ideal to accommodate out-of-town patients. Delightful hotels are conveniently close and many couples vacation at the world’s most beautiful beaches during their visits.
Patients can read about personal experiences of other women who had this surgery for infertility on our “People Sharing Their NewLIFE Experiences” webpage.
*Actual cost may vary for some patients based on location, and an individual’s need for medications and other services.
Conceiving with Donated Eggs
Oocyte (egg) donation, available since the mid-1980’s, and has become the most effective option for women with low “ovarian reserve” or early/premature menopause, or some with severely poor egg quality. The process involves harvesting oocytes from the ovaries of a woman with normal fertility and egg numbers (the “egg donor”). These eggs are fertilized with the sperm of the intended father and then, the resulting embryo(s) are transferred into the uterus of the intended mother. If pregnancy is established, the mother then becomes the “gestational” mother and experiences the pregnancy and birth, although she is not the genetic mother. Her partner providing the sperm is the genetic father. The entire process has been made easier with the advancement of “egg freezing”. Eggs may now be cryopreserved and shipped to the site of use, similar to the ease of procuring semen for donor insemination. NewLIFE assists women in the process after selecting donor eggs from domestic Donor Egg Banks. The donor’s characteristics are matched for the receiving woman’s personal preferences. An additional advantage of the egg banking process is the lower cost of using donated eggs, making this more affordable for many. If you are interested in discussing this wonderful option, please submit a request to become a new patient at NewLIFE.Egg Cryopreservation
Freezing (Cryopreservation or “Cryo”) of living cells has been successfully used in research laboratories for many years, and increasingly, in veterinary and human reproductive medicine. The first birth results after the freezing and thawing of a human embryo occurred in Australia in 1985 and the number of reported deliveries from the transfer of previously cryopreserved embryos has increased steadily in the United States. Techniques for cryopreservation of eggs (oocytes) have advanced rapidly allowing the retrieval and storage of unfertilized eggs for later use in reproduction. Eggs that are cryopreserved with these newer techniques have high survival rates. The woman’s age, of course, factors significantly into the quality and outcome with cryopreserved eggs. Experience with eggs from young donors is reassuring. Eggs retrieved and thawed years later can be fertilized with a partner’s sperm using standard Assisted Reproductive Technologies (ART). There are many situations where a woman may desire fertility preservation. Most commonly in modern society, family planning is being delayed to find the right partner, and for completion of education, starting of careers and a desire to spend more time as a couple before becoming a family. Also, cancer in young women may require chemotherapy or radiation therapy that can reduce or completely damage viable eggs. In these instances, eggs can usually be retrieved within a 1-2 month period before cancer treatment.Various reasons that women consider egg cryopreservation;Patients can read about personal experiences of other women who had this surgery for infertility on our “People Sharing Their NewLIFE Experiences” webpage. If you are interested in discussing this special option with our expert providers, please submit a request to become a new patient at NewLIFE.
- Desiring to delay childbearing until after age 30-35
- A type of cancer that will require chemotherapy and/or radiation
- A history of early menopause (before age 45) in family members
- Advanced stage or aggressive endometriosis confirmed in a prior surgery
- Concern about ovarian reserve after multiple ovarian surgeries for cysts and tumors
Male Fertility Services
Semen Analysis
Semen analysis (SA) is often the first step in evaluating male fertility and helps providers determine the most appropriate path to pregnancy. The analysis assesses sperm count (concentration), movement (motility), and shape (morphology), and the results help guide care options ranging from natural conception to assisted reproductive treatments such as intrauterine insemination (IUI), in vitro fertilization (IVF), or intracytoplasmic sperm injection (ICSI).
NewLIFE offers semen analysis for couples who are actively trying to conceive, with testing scheduled as part of the new couple work-up. Testing is performed by the Andrology Laboratory by appointment only. A male presenting without a partner must have intent to conceive and provide a signed doctor’s order for a semen analysis from another physician in order to establish care and schedule testing. Individuals without a referral may be assisted with access to testing through Fellow or another external consumer testing service.
NewLIFE does not provide semen analysis for general screening, curiosity testing, or to confirm sterility after vasectomy.
Please contact our office if you have any questions regarding specimen collection parameters, payment, and the process.
Male Hormone Testing
Hormonal testing of the male can help fertility specialists pinpoint conditions that may be contributing to their inability to conceive.
Testosterone and various hormones made in the brain control sperm production. When an abnormal level of these hormones is discovered, specific therapies may be chosen. Hormonal dysfunction in men remains one of the uncommon, but treatable, causes of low sperm production. Consistent with our philosophy at NewLIFE, we prefer to evaluate the male also, to avoid delays and to manage the couple for best outcomes. Thus, it is a routine recommendation for the male to be present and be authorized for consultation along with the female.
Male Genetic Testing
“Male factor infertility” is the name for any condition in the man that may be a reason why a couple cannot have a baby. Certain conditions can increase these chances.
Our fertility specialist may recommend genetic testing if you have one or more of the following conditions:
- Very low sperm count, or no sperm seen in the semen
- Physical features that suggest a genetic cause
- Several miscarriages
The chances of identifying a genetic cause for male factor infertility depends on the man’s laboratory results, physical exam findings, ethnic and racial background, and family history.
What genetic tests are recommended for men with male factor infertility?
The three most common genetic tests are:
- Karyotype (chromosome analysis)
- Y chromosome microdeletion test
- Cystic fibrosis (CF) gene test
Increasing Sperm Production
Men who are attempting to conceive but who are found to have “low sperm counts” require detailed testing in an attempt to identify a specific cause. When the cause remains unknown and techniques are applied to utilize the current low counts. In other cases, sperm production can be increased over 2-4 months using fertility stimulating medications.
For men who have effective sperm-making machinery, the addition of medications will sometimes allow the natural increase in sperm production. Sperm requires 2-3 months to fully mature, so the treatment takes time, but in properly selected cases, this approach can be quite helpful, sometimes allowing for spontaneous conception.
There are always general recommendations for men with low sperm production that may be helpful toward improvement. These approaches include:
- Eating a healthy diet, rich in anti-oxidants.
- Maintaining a healthy weight.
- Avoiding excess alcohol and tobacco exposure.
- Increasing physical activity.
Semen Cryopreservation
When sperm is obtained for future reproduction, such as for men planning vasectomy or chemotherapy, NewLIFE assists in coordinating the cryopreservation and the long-term storage arrangements. This approach is also useful when the male’s availability at the time of ovulation is uncertain. Military personnel who deploy on short notice are examples where cryopreservation can avoid a prolonged delay in treatment or attempted conception.
Alternatives to Vasectomy Reversal
Men considering vasectomy reversal should also consider the alternative of direct sperm retrieval (without vas reversal) and should consult with an experienced fertility specialist who will discuss the advantages of BOTH approaches. Obtaining the most up to date information on outcomes and costs will help in selecting the best option for a couple’s unique circumstances.
The length of time since vasectomy is an important factor. With vasectomy more than 5 years duration, the chances of a successful conception and delivery decrease. This becomes particularly important when the female is over 30 years of age as sperm counts may not recover immediately.
To conceive after vasectomy, sperm retrieval is usually completed in an office setting, as with the original vasectomy, without the need for general anesthesia. There is no need for incisions or stitches with sperm aspiration and men return to routine activity quickly.
OUR eBOOK
Thinking about Freezing Your Eggs? Learn What to Expect
Egg freezing at NewLIFE is more than a medical procedure — it’s a way to take control of your future with clarity, compassion, and confidence. Complete the form below to get a copy of our free egg freezing ebook to learn more.