Obesity and Fertility
Many health factors affect fertility, conception and healthy pregnancy. A woman’s body seems to protect or prevent pregnancy when not in good health. Think about women whose menstruation stops when exercising excessively or with poor diet. Women considering or planning a pregnancy will benefit by preparing in advance and by being as healthy as possible before conception. This will reduce the chance of complications, including infertility. One clear example is tobacco smoking, which has been shown to delay conception. It takes longer to become pregnant when smoking. And worse, smoking affects a woman’s “ovarian reserve,” causing the number of eggs to decline faster.
While it is always a personal, and sometimes a sensitive subject, excess weight and obesity also appear to delay pregnancy in some women (and men), particularly those with a family history of diabetes. Obesity will also increase the chance of severe complications during a pregnancy, such as high blood pressure, diabetes and delivery complications. Though a delicate topic, if fertility physicians avoid its discussion, they would be denying patients an opportunity to improve their chances of faster and successful pregnancy. It shouldn’t be a shame to be overweight, but it is unfortunate if patients aren’t given information that can help.
Measuring the Fertility Impact
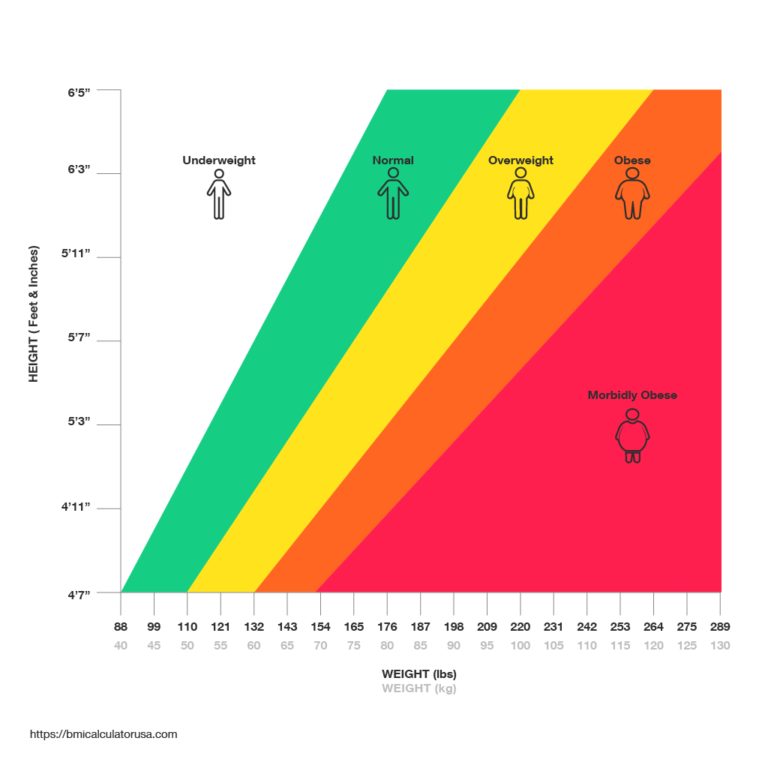
Obesity is defined by Body Mass Index, “BMI.” BMI was developed as a measure of health and longevity. Overweight is defined as BMI 26-29, and obesity is BMI >30. The exact way that high BMI affects fertility is uncertain but it appears to affect egg quality and embryo implantation. This effect is clear when looking at the Society for Assisted Reproductive Technologies prognostic website. The user can enter her personal information and based on hundreds of thousands of IVF cycles in the United States, the site will provide an estimate for successful “live birth”. Using this consumer resource (SART Predictor), for every increase of 5 units in BMI >30, a woman’s chance of pregnancy declines by 3-5% per attempt.
Steps That Patients Can Take to Guide and Help with Weight
Women with a BMI >30, irregular menstrual periods, or symptoms of “PCOS” should seek medical evaluation, testing to see if weight has affected menstrual periods, fertility and/or metabolism. A Reproductive Endocrinologist is uniquely qualified to assess these, while an Ob/Gyn may not. Once testing is complete, if problems are identified, the specialists can make recommendations, sometimes medications that will improve the abnormal findings, improve overall health and well being, AND raise the chances of a health pregnancy. Let’s talk!